Reimbursement Claim in Health Insurance
A reimbursement claim in health insurance is when you pay for your medical treatment out of pocket and later submit a claim to your insurer to get that money back.
This type of claim is typically used when you receive treatment at a non-network hospital or in situations where cashless services aren’t available. While it requires you to handle the hospital bills initially, the insurer reimburses you for eligible expenses once you submit the necessary documents and the claim is approved.
I agree to the Terms & Conditions
Get Exclusive Porting Benefits

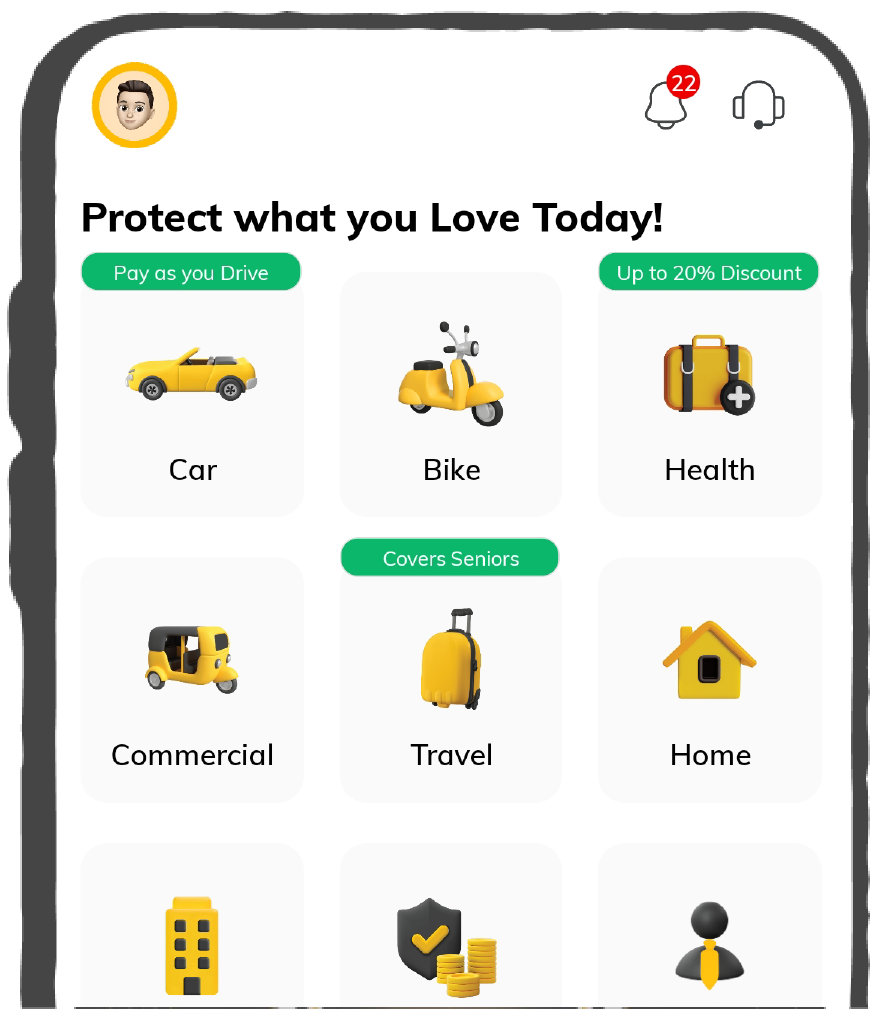
Buy Health Insurance, Up to 20% Discount
Port Existing Policy
9000+
Cashless Hospitals
2.5 Crore+
Lives Insured
4.5 Lacs+
Claims Settled
Meaning of Reimbursement Claim in Health Insurance
A reimbursement claim is an official request for compensation or a refund for out-of-pocket medical expenses made by a policyholder to their health insurance policy provider.
In simple words, a Reimbursement Claim is a type of claim in which an insured must pay for medical costs and treatment out of their own pocket and later claim the bill from the insurance provider. For this kind of claim, the insured can visit any hospital for treatment, not necessarily the empanelled cashless hospital.
Let’s understand this with an example:
Shweta has a health insurance policy and resides in Delhi. She had to undergo a minor nerve surgery, for which she visited her family neurosurgeon. Unfortunately, the hospital she chose was not empanelled with the insurance company. 😣
After treatment, she paid the treatment cost herself and kept all the essential documents, invoices and receipts. She filled out a reimbursement claim for the insurance company and after verification, her expenses were returned to her. 🙂
Benefits of a Reimbursement Claim in Health Insurance
How Does the Reimbursement Claim Process Work?
A reimbursement claim works by allowing you to pay for your medical treatment upfront and then recover the eligible expenses from your health insurance provider. Here's a step-by-step explanation of how it works:
Get Treated at Any Hospital
Select any hospital (whether within a network or not) for treatment.
Pay & Keep the Bills
Settle all medical expenses upfront from your own pocket and keep the bills or invoices, such as those for doctor’s consultations, diagnostic reports, and hospital bills.
Submit a Claim to the Insurer
Complete the claim form and submit it along with the required supporting documents.
Claim Review & Verification
The insurer reviews your documents to verify the treatment, expenses, and policy coverage. They may request additional documents if necessary.
Approval and Reimbursement
Once approved, the insurer reimburses the claim amount directly into your registered bank account.
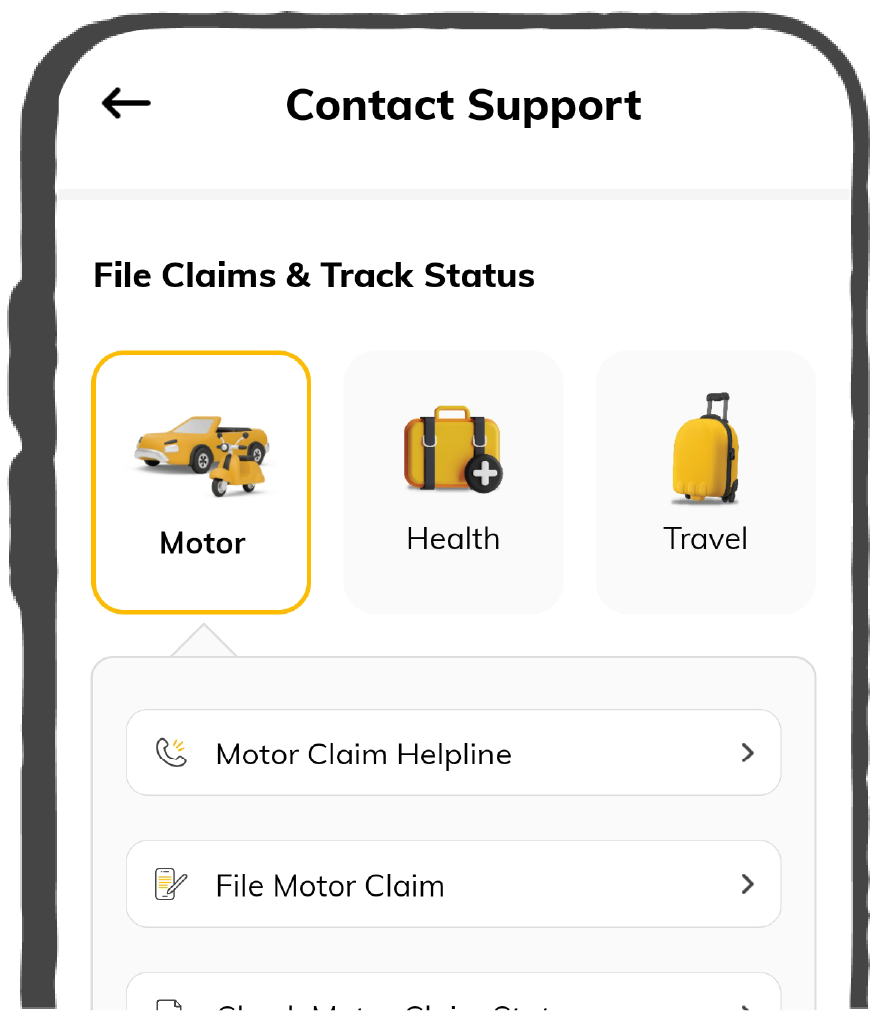
How to File a Reimbursement Claim at Digit?
Get Treated & Save Everything
Visit any hospital, pay the bills upfront, and collect all the necessary documents (bills, reports, prescriptions, discharge summary, etc).
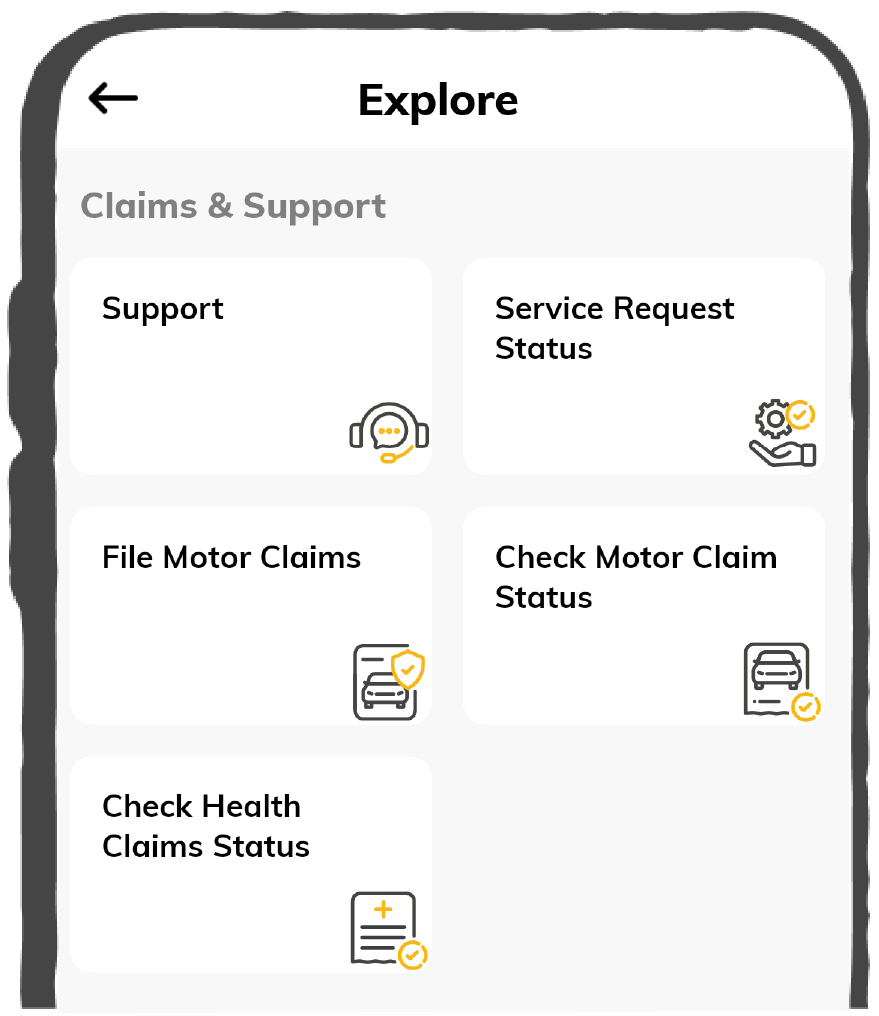
Open Digit App & File Claim
Log in to the Digit App. Navigate to the ‘File a Health Claim’ section on the app. Choose the policy, enter your details and & type of claim (reimbursement claim).
Enter Details & Upload Documents
Fill out additional details of treatment, symptoms, hospital details, etc. Scan and submit all the necessary documents in the desired format.
Register Claim & Relax
Click ‘Register Claim.’ We’ll review everything, and once approved, the amount will be reimbursed directly to your bank account.
Documents Required for Reimbursement Claims
When filing a health insurance claim, you need to submit certain documents to ensure a smooth and hassle-free process. Below is a list of essential documents that may be required while filing a reimbursement health claim at Digit:
Hospitalisation Documents
Cashless Documents
KYC Documents
When Should You File a Reimbursement Claim?
A reimbursement claim becomes necessary when you’ve paid for medical expenses out of pocket and must recover the costs from your insurer. This often happens when treatment is done at a non-network hospital in India, where cashless facilities are unavailable.
Additionally, expenses such as pre and post-hospitalisation costs, diagnostic tests, and outpatient treatments that aren’t covered under cashless claims may require reimbursement filing.
Let’s take different cases and understand which claim you should file in which situation:
Scenarios |
Type of Expense |
Type of Claim to File |
You went for planned surgery in a network hospital where the insurer settles the bill directly with the hospital. |
Hospitalisation |
Cashless Claim |
You had to undergo emergency surgery at a non-network hospital, where you had to pay the bills. |
Hospitalisation |
Reimbursement Claim |
You needed immediate hospitalisation due to an accident. |
Accidental Hospitalisation |
Cashless Claim (network hospital) and Reimbursement Claim (non-network hospital) |
You underwent surgery in a network hospital in India, but your cashless claim was rejected due to missing documents. |
Hospitalization |
Reimbursement Claim |
You had to undergo a consultation and lab tests weeks before and after getting hospitalised for a medical procedure. |
Pre & Post-Hospitalisation Claim |
|
You had to visit a clinic weekly for skin allergy treatment without requiring hospitalisation. |
OPD Expenses |
Reimbursement Claim |
Factors to Consider Before Filing a Reimbursement Claim
Medical reimbursement claims might be a good option, considering the flexibility they provide in terms of selecting the medical centre for treatment. We can choose any desirable hospital, not just the empanelled hospital.
However, while opting for a reimbursement claim or selecting a non-network hospital, one must consider a few points as listed below:
Reasonable and Customary Charges under Reimbursement Claims
For both network and non-network hospitals, reasonable and customary charges, which are the standard charges for a specific provider and consistent with prevailing charges in the geographical area for identical or similar services, taking into account the nature of the illness /injury involved, and which are medically necessary, will be considered for payment of admissible claims.
In case treatment is received at a Network hospital, payment of claims will be as per Digit’s pre-negotiated rates with the hospital and in case treatment is received at a non-network hospital, reimbursement will be limited to rates applicable at par with another comparable network hospital.
Common Reasons for Reimbursement Claim Rejection
This may sound unusual, but there are several reasons why claims can be rejected. It can be due to either documentation or incorrect information. Let’s discuss the common reasons why your claim can be rejected:
- Insufficient Documentation: Bills, invoices, and medical records are missing or incomplete, which may result in a claim being denied.
- Exclusions from the Policy: Certain treatments may not be covered, depending on the terms and conditions of your policy.
- Waiting Period Not Over: Especially in health insurance, some conditions have a waiting period before claims can be made. According to Digit’s Transparency Report, around 8% of health claims were rejected mainly due to waiting periods.
- False Information: Your claim form may only be accepted if you provide correct or sufficient information.
- Non-payment for the Policy: Any claims made during this time may be denied if your coverage has lapsed due to non-payment of premiums.
What to Do if Your Reimbursement Claim is Rejected?
Don't freak out if your reimbursement claim is denied. You can re-apply for a claim if the claim is rejected because of documentation. Here are some ways you can deal with claim rejections with the following actions:
- Examine the Notice of Rejection: Please examine the notice of rejection that your insurance company sent you carefully and recognise the precise justifications for the rejection.
- Speak with Your Insurance Company: Ask your insurance company for more information. Request clarification on the reasons for the rejection and advice on the next course of action.
- Review the Policy Coverage Twice: Verify that your policy paperwork accurately reflects the costs you reported. Misunderstandings or misinterpretations can occasionally lead to rejections.
- Fix Any Mistakes: Correct any mistakes in the original claim filing as soon as possible.
- Obtain Medical Advice or Records: If the rejection was caused by a disagreement regarding the necessity of the therapy, consider getting a second medical opinion or acquiring more supporting paperwork from your healthcare provider.
- Follow up Continuously: Throughout the appeals process, communicate continuously with your insurance carrier and record every conversation.
Digit’s Health Insurance Claim Numbers for FY 2024-25
Interesting Claim Stories about Digit Health Insurance
You might have understood by now that reimbursement claims in health insurance offer a reliable solution for managing medical expenses when cashless facilities aren’t an option.
Understanding the process and ensuring all required documentation is in place can help you easily reclaim your financial outlays. This is crucial to ensuring comprehensive health coverage, giving you peace of mind and allowing you to focus on what truly matters—your recovery and well-being.